The pelvic floor is a complex group of muscles, ligaments and fascia that supports the pelvic organs (bladder, uterus, rectum) and helps regulate functions such as urinary continence, bowel control and sexual intimacy. Over time and under various stresses, this system can malfunction — a condition commonly referred to as pelvic floor dysfunction (PFD). In women this may manifest as:
- Urinary incontinence (stress, urge or mixed)
- Pelvic organ prolapse (uterus, bladder or rectum descending)
- Sexual dysfunctions (pain, decreased sensation, difficulty / incontinence during intercourse)
- Pelvic pain, hip or sacro-iliac dysfunction, bowel urgency or constipation
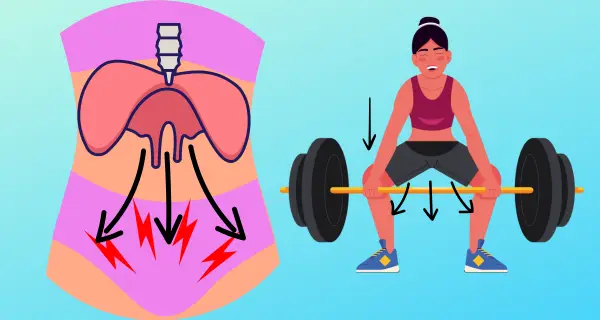
There are many contributing causes including pregnancy/childbirth, menopause (with associated hormonal changes such as vaginal dryness and tissue thinning), chronic coughing or constipation, obesity, heavy lifting, high intra-abdominal pressure (IAP), poor posture and a weak or uncoordinated pelvic floor/abdominal/diaphragm system.
Recent evidence emphasises that excessive or poorly controlled intra-abdominal pressure (IAP) is a strong predisposing factor for PFD: one randomized controlled trial observed the link between IAP, breathing mechanics and pelvic floor health. (MDPI)
In the menopausal transition, decline in oestrogen and collagen support leads to tissue thinning, vaginal dryness, decreased pelvic floor muscle (PFM) responsiveness and increased risk of incontinence or prolapse. That makes it especially important for women in this life-phase to adopt preventive and rehabilitative strategies.
Why Posture, Breath & Core Integration Matter
When we look at PFD not just as “weak pelvic floor muscles” but as a system dysfunction involving diaphragm, deep abdominals, pelvic floor, posture and breathing, we unlock greater potential for meaningful improvement. Key elements include:
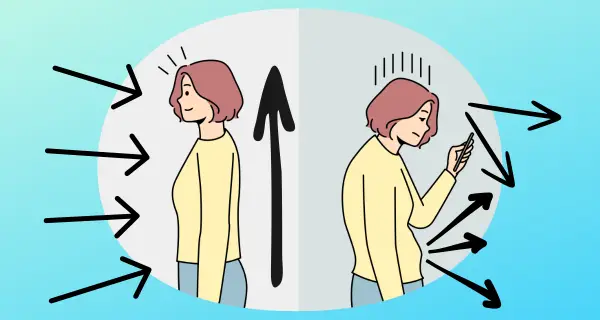
- Postural alignment: A collapsed rib cage, forward head, shoulders rounded, or excessive lumbar curve all influence the way the abdominal wall, diaphragm and pelvic floor behave under load.
- Diaphragm-pelvic floor synergy: On inhalation the diaphragm descends, on exhalation it ascends, this movement interacts with the pelvic floor. Dysfunctional breathing or postural collapse can lead to elevated intra-abdominal pressure and inefficient pelvic floor responses. (MDPI)
- Intra-abdominal pressure (IAP) control: Activities like heavy lifting, chronic constipation, coughing or even high-impact exercise increase IAP repeatedly. If the pelvic floor cannot respond or the system is mis-aligned, that pressure gets transmitted to pelvic organs and fascia rather than being managed by coordinated contraction/relaxation.
- Core and pelvic floor synergy: Deep abdominals (transversus abdominis), multifidus, pelvic floor, diaphragm and the fascial sling work together. Poor activation, poor timing or poor posture = inefficient system. A 2021 RCT found that eight weeks of hypopressive (abdominal) training improved postural control and deep trunk muscle activation. (PMC)
In short: if posture is collapsed, breathing is shallow or dysfunctional, and the core/pelvic system is not integrated, you will likely carry more strain, pressure and dysfunction in your pelvic region.
The Evolved Role of the Hypopressive Method
The method of abdominal hypopressive training (AHT), originally developed by Marcel Caufriez in the 1980s, has recently undergone significant evolution. It’s no longer just about “opening the rib cage” or “holding breath with ribs lifted”. Today we understand it as a postural-breathing-core integration system.
Key shifts to highlight:
- Original concept: The early work emphasised rib cage expansion (the “rib lift”), voluntary apnea (breath hold) and abdominal vacuum to reflexively recruit pelvic floor muscles (PFMs).
- Modern understanding: Research now emphasises postural alignment, diaphragmatic breathing, fascial line integration, reduction of excessive IAP, and automatic reflex activation of the PFMs, rather than purely voluntary or isolated PFM contraction.
- Misconceptions to correct: Some practitioners still teach hypopressives as “just open the ribs, hold breath, contract the belly and lift the PFMs”. That is outdated. Without correct posture, breathing pattern, fascial alignment and timing, the technique may not yield the intended benefits.
- Research evidence:
- A systematic review (2024) found hypopressive exercises show positive effects on abdominal and pelvic floor muscles in women, but emphasises the need for high-quality clinical trials. (Bodywork Movement Therapies)
- A 2023 RCT found that eight-week hypopressive training significantly improved PFM activation, load absorption and muscle efficiency in women with mild-to-moderate PFD. (Wiley Online Library)
- Another 2020 RCT (J. Clin. Med. 2020;9:1149) showed benefits of hypopressives in women with PFD. (PMC)
- But, some research (2024 abstract) found eight weeks of hypopressive training did not change PFM strength or stiffness in healthy women, suggesting the effect may depend on baseline dysfunction and quality of instruction. (CS)
What this means clinically: Hypopressive training is promising as part of an integrated rehabilitation/postural system, particularly in women with PFD, postpartum changes, or those entering menopause. It is not a magic pill and must be taught correctly with posture, breathing, core control and guidance.
How Hypopressive Training Helps with PFD (and Women’s Health)
By emphasising posture, breath control, core/pelvic-floor synergy and reduction of excessive IAP, hypopressive training can address key mechanisms of PFD:
- Reduced intra-abdominal pressure load: By training movement patterns that manage IAP rather than repeatedly load the pelvic floor and abdominal wall. This lessens strain on the pelvic floor, important in preventing urinary incontinence and prolapse.
- Improved postural alignment: A more upright, aligned rib cage-pelvis relationship changes mechanics so that the abdomino-pelvic complex works more efficiently rather than being in overload.
- Reflex pelvic floor activation: Modern hypopressive training aims to engage the pelvic floor reflexively (via breath/diaphragm/abdominal synergy) rather than through isolated “Kegels” alone. For many women with poor proprioception or low awareness of the PFMs (e.g., after childbirth or menopause) this can be a more accessible entry.
- Core-diaphragm-pelvic floor integration: Because the diaphragm, transversus abdominis and pelvic floor work as a unit, training this synergy improves stability, reduces leaks, and improves sexual function and organ support.
- Support through menopause: As women transition through menopause, thinning tissues + changes in biomechanics + hormonal shifts increase the risk of PFD. Hypopressive training offers a non-hormonal, movement-based approach to maintain tone, improve posture and support pelvic health.
- Sexual function & vaginal health: Although direct research is less abundant here, improved pelvic floor tone, posture and alignment can contribute to better sexual responsiveness, decreased dyspareunia, and general pelvic comfort. Incorporating breath and posture also helps the nervous system calm and integrate, which matters in sexual health.
Why Choose Certified, Modern Hypopressive Guidance
Because the method has evolved, it’s crucial to work with a therapist who is certified by Marcel Caufriez and follows the latest evidence-based approach. At Chaux Physical Therapy we are proud to offer this:
- Our hypopressive training integrates modern posture, breath and core-pelvic floor synergy (not just rib lift).
- We use protocols rooted in current research (2020-2024) and tailor the work to women’s lifecycle stages (postpartum, menopausal, PFD recovery).
- We emphasize correct alignment, diaphragm-pelvic floor synchrony, fascia and movement quality, so you don’t just “exercise” your pelvic floor, you retrain your system.
- We offer virtual sessions, one-on-one private sessions, and now semi-private hypopressive sessions (max 4 people), providing a supportive group environment while still maintaining personalised feedback and technique correction.
- You’ll learn not only how to do the technique, but when to use it (in daily life, posture, movement), how to reduce excessive IAP in daily tasks, how to integrate it into holistic pelvic health (including managing menopause changes: dryness, decreased tone, postural shifts).
What You’ll Get and Why It Works
Here’s how we deliver the service and why it makes a difference:
- Initial assessment: We evaluate your posture, breathing pattern, abdominal-pelvic floor coordination, history (childbirth, menopause, incontinence, prolapse symptoms) and set goals.
- Private hypopressive coaching (virtual or in-person): You’ll learn the modern hypopressive sequence, posture corrections, breath timing, core-pelvic alignment.
- Semi-private hypopressive group (4 persons max): A small-group environment with coaching and corrections, ideal for women comfortable being in the company of others working on similar goals.
- Integration into daily life: Training includes how to apply these techniques into movement, lifting, carrying, coughing, posture breaks, pelvic health tasks, so you’re not just doing “exercise”, you’re rewiring how your system handles pressure and load.
- Lifecycle focus: Whether you’re postpartum, perimenopausal, menopausal, or beyond, we incorporate relevant modifications to support your body’s unique stage of life, addressing vaginal dryness, hormonal shifts, tissue changes, and biomechanics. In addition, we include guidance on sleep habits, stress management techniques, proper hydration, and nutrition with an anti-inflammatory focus to help you restore balance and enhance overall well-being.
- Follow-up & progression: We track your improvements (continence, alignment, pelvic symptoms, functional movement) and adjust accordingly.
Key Evidence to Support Hypopressive Training in Women with PFD
- The RCT by Navarro-Brazález et al. (2020) found hypopressive exercises produced improvements in women with PFD. (PMC)
- The recent systematic review by Katz et al. (2024) supports that hypopressive exercises positively affect abdominal and pelvic floor muscles in adult women, though more high-quality trials are needed. (Bodywork Movement Therapies)
- The 2023 RCT (Molina-Torres et al.) found that an 8-week hypopressive program significantly improved PFM activation and load absorption in women with urinary incontinence and PFD. (Wiley Online Library)
- A 2024 study (Herena-Funes et al.) looked at ventilatory mechanics and quality of life after 8-week hypopressive training, again emphasising the diaphragm-pelvic floor link and the postural/respiratory mechanics. (MDPI)
- Note: Some studies (e.g., Saraiva et al. 2024 abstract) found no change in PFM strength after 8 weeks in healthy women. This suggests that population (healthy vs dysfunctional) and quality of instruction matter. (ICS)
Taken together: there is a growing but still evolving evidence base indicating that hypopressive training (when correctly applied) can be a valuable tool in women’s pelvic health, especially as part of integrated physical therapy and not just isolated exercises.
Why This Matters for You
As a physical therapist and women’s health specialist, Chaux Physical Therapy focuses on restoring mobility, calming the nervous system, integrating body-mind connection and healing the whole person, especially in contexts such as irritable bowel syndrome, post-cancer therapy, and pelvic floor dysfunction. The inclusion of hypopressive training aligns perfectly with those goals because it addresses posture, breath, core-pelvic coordination; not just “strengthening” but realigning and re-educating the body to work with less effort and less abnormal pressure.
When your core-pelvic system works with less effort, your pelvic floor can function with less strain, which is exactly what we want: less leaking, less heavy feelings, less prolapse stress, better sexual function, improved posture and decreased pain.
What’s Next and Invitation
If you’re experiencing any of the following: urinary leakage when sneezing/coughing/exercising, heaviness in the pelvic region, a sense of “dropping” or pelvic organ shifting, pain or discomfort during sex, or simply want to be proactive (especially as you approach or are in menopause), the next step is to work with someone who understands the whole system.
You are warmly invited to schedule a virtual session or book a private in-person session at Chaux Physical Therapy. We’re also offering semi-private hypopressive sessions (max 4 women) which combine personalized instruction. Together we’ll assess your posture, breathing, pelvic-core coordination, then teach you how to use hypopressive training correctly, in its modern form, aligned with the latest evidence and your unique body.
In Summary
- Pelvic floor dysfunction in women is common, urinary incontinence, prolapse, sexual difficulty, and often driven by weak coordination of posture, breath, core/pelvic floor, and high intra-abdominal pressure.
- Modern hypopressive training evolved from the original work of Dr. Marcel Caufriez emphasizes the synergy between posture, breathing, and core/pelvic floor activation, rather than simply focusing on the traditional “rib lift and breath hold.” Dr. Caufriez’s continued research and extensive clinical experience have deepened his understanding of the hypopressive method, leading to its ongoing evolution. He is now sharing this advanced, evidence-informed approach with professionals and practitioners worldwide.
- Emerging evidence (2020-2024) supports its use in women with PFD, especially when taught correctly and integrated into a broader rehabilitation/postural approach.
- At Chaux Physical Therapy we offer virtual, private and semi-private hypopressive sessions tailored for women’s health, including those in menopause, postpartum, or recovering from pelvic floor dysfunction.
- If you’re ready to improve your pelvic floor health, improve posture, reduce pressure load, enhance sexual health and regain confidence, this is your invitation.
Modern Hypopressive training offers a postural, evidence-based way to support pelvic health at every stage of life.
At Chaux Physical Therapy, we’re proud to bring this evolving method, as certified by its creator, Marcel Caufriez, to women seeking lasting solutions for pelvic floor dysfunction.
We welcome you to explore our virtual, private, or semi-private sessions and experience a smarter, gentler way to restore your pelvic health.